Sometimes reiteration makes tasks look harder.
Celladon recently reiterated the case for Mydicar, their AAV1-SERCA2A therapy for patients with heart failure with reduced ejection fraction (HFrEF), at the BioCEO gathering. Celladon has come to prominence based on a subgroup analysis of their CUPID1 trial, wherein the Mydicar high dose arm (n=9) showed statistically significant improvement over the placebo arm (n=14). Although some are convinced by this study result, I’ve expressed my skepticism in an earlier post. Unfortunately the recent presentation makes the Mydicar proposition look less likely to succeed.
In the earlier piece, I’d highlighted strong reasons to question the degree of cardiomyocyte transduction and SERCA2A expression induced by Mydicar therapy. Celladon’s CEO was much more upbeat at BioCEO, describing the administration as one that results in “homogenous uptake” resulting in SERCA2A being expressed “for the life of the cell.” Perhaps that’s a form of confidence in the product. Unfortunately, their data to date provide little support for such unequivocal claims. The discrepancy between the presented scientific data and the company’s claim can be a red flag in and of itself: it is one thing to be confident in your program, but it is more effective if that confidence isn’t accompanied by claims that seem to be undermined by your own published data.
Rather than getting bogged down in the details of the AAV1 mechanism and SERCA2A protein expression, another way to assess this program is to examine the upcoming clinical trial expectations and compare them to historical observations. Celladon is currently running CUPID2, their sequential follow-up to CUPID1. CUPID2 is placebo controlled and enrolling 250 patients (~86% NYHA Class III/IV) split evenly into two arms. Participants will receive the high dose of Mydicar that resulted in statistically significant improvement for 9 patients in CUPID1 compared to their 14 placebo / best available care comparators. In this subgroup analysis, CUPID1 demonstrated an 88% risk reduction. That’s a very large number, especially when compared to our current and upcoming standards of care. To note:
- Beta-blockers provided a 19% risk reduction in a HFrEF population that was ~60% NYHA class III/IV
- LCZ696, the new offering from Novartis, provided a 20% risk reduction in a HFrEF population that was ~30% NYHA class III/IV
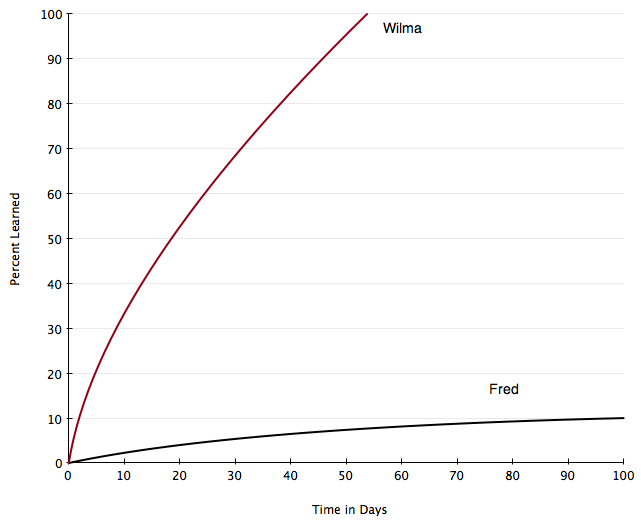
In these multi-thousand patient trials, two drugs, one a mainstay and the other a hopeful newcomer to heart failure treatment, have shown ~20% risk reductions. The trials did not enroll identical patient populations, but nonetheless the risk reduction percentages are eerily similar. In that light, CUPID1’s 88% risk reduction can either appear stellar, or more convincingly a fluke event. It is hard to imagine that this treatment will come out with a risk reduction that is four times those observed in these large trials. This is especially difficult to reconcile since we know that the SERCA2A mechanism of action overlaps with the beta-blocker mechanism of action. In fact, preclinical models have demonstrated that beta-blocker treatment can restore low SERCA2A expression, which is Mydicar’s raison d’etre. If beta-blockers, within their broader mechanism of action, increase SERCA2A expression the way Mydicar is proposed to, is it reasonable to expect that Mydicar demonstrate a risk reduction that is twice as large as that for beta-blockers?
It is not controversial to state that the risk reductions in larger trials tend to be smaller than those in earlier, smaller, proof-of-concept trials. Celladon’s design of the currently running CUPID2 trial suggests that they’re aware of this contributing factor, as the trial was designed to have 83% power to detect a 45 percent risk reduction. This is a more modest target, and the results are due in April, 2015. The company concedes that they need a p value significantly less than 0.05 to make this trial the primary basis of approval. At the same time, the company appears to concede that CUPID2, in and of itself, is unlikely to support registration. They note that a follow-on trial, CUPID3, is under planning and will be used as a phase 3 or phase 4 trial, depending on CUPID2 results and their conversations with US and European regulators.
In effect, for CUPID2 to form the primary basis for registration of Mydicar, the 250 patient trial needs to have an outcome that would come close to replicating the 80%+ risk reduction seen in a 23 patient subgroup analysis. That is a tall order for any drug.